
When Dr Morrie Shapiro first made the move to help set up a first ever general intensive care unit at a small hospital in Netanya Israel, he could never have imagined that 20 years into the future, in today’s world, that a global pandemic would strike.
It almost seemed the stuff of science fiction. The world didn’t have plans or protocol in place for a pandemic of such magnitude and that is why COVID-19 put such massive and unanticipated pressure on the hospital’s resources. All the while, it was the ICU team that was at the forefront of managing this crisis.
The novel virus’ unusual immune-inflammatory response meant that it evolved with a uniquely challenging set of characteristics that makes it incredibly difficult to treat.
Despite all the difficulties and the dangers presented by the virus, the Laniado ICU team rose to the challenge and treated hundreds of severely ill COVID-19 patients.
“We were blessed to have many successes, where we were able to return many severely ill patients back to their homes and to their families to continue normal, healthy lives.”
Morrie credits the nursing staff for the selfless care they provided to patients and their families which contributed to the entire team functioning like a well-oiled machine.
Unfortunately, there were patients who failed to respond to our intensive treatment. These patients of course were kept comfortable and our amazing team of nurses and social workers proved a tower of strength in supporting the families during this most difficult of times.
From the perspective of a hospital on the front line, to help give a clearer idea of the difficulties that were faced and are still being faced because of this evolving virus, I would like to share the story of David, a Netanya resident.
David began having breathing trouble in March of 2020 and was admitted to Laniado Hospital.
He was in his late sixties and had been recently treated for cancer. As a result of the chemotherapy and radiation treatments his immune system was severely compromised. As his condition deteriorated, he had to be placed on a mechanical ventilator and was transferred to the general ICU.
David gradually stabilized and there was even a suggestion of improvement in his condition but on the third day he began to drastically deteriorate and we were unable to oxygenate which put him in a precarious position. A low concentration of oxygen in the blood is extremely dangerous, potentially irreversible and can cause permanent organ damage. “Our patient was dying in front of our eyes!”
We were blessed to have many successes, where we were able to return many severely ill patients back to their homes and to their families to continue normal, healthy lives.
Dr Morrie ShapiroLaniado Hospital
In order to save his life we had to immediately find the cause of the problem so that we could provide lifesaving treatment. Emergency blood tests and x-rays were unsuccessful. An echocardiogram revealed stress on the right side of the heart. Amongst the possible causes of right sided heart strain, is a blood clot in the lungs.
At that stage, during the first wave of the pandemic, it was not clear whether COVID-19 was capable of causing a hypercoagulable state in the body - an increased tendency of blood to clot - which could lead to a pulmonary embolism. The diagnosis of a pulmonary embolism is usually made as a result of a CAT scan but David was too sick to be moved to the CT suite.
Treatment for a pulmonary embolism, causing severe respiratory and hemodynamic problems, involves giving a potent drug that dissolves the clot. The problem with this is that the drug is so potent that it may result in severe bleeding in various parts of the body including the brain. Instead of helping the patient, by giving this medicine, you may cause irreparable damage to the patient – sometimes even resulting in death.
Nonetheless, after taking all the many factors into consideration, our team decided to administer the drug. Within minutes, David's condition began changing. His blood pressure increased and the concentration of oxygen in his blood improved significantly.
However, David was not out of the woods yet. A week later he contracted severe pneumonia which led to cardiac arrest. It was only due to the rapid intervention of the ICU team that he was able to survive this crisis as well.
David continued to improve. He woke up without any evidence of brain dysfunction.
After a stay of five weeks in our intensive care unit we were able to wean him off the ventilator and he was transferred to the Beit Levenstein Rehabilitation Hospital where he continued to improve and was finally discharged in good condition.
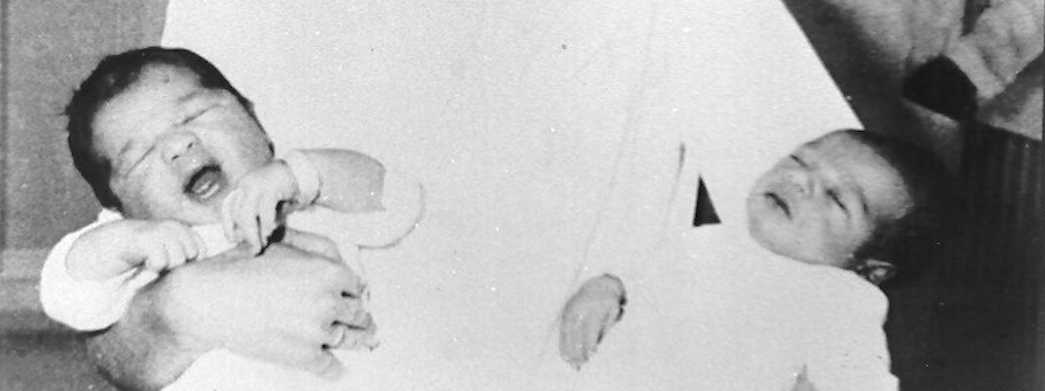
Today David is completely independent. He is able to drive a car and a few months ago he had the honour of being the sandek at his twin grandsons Britot Mila - a truly inspiring story.
David’s story is one of thousands of severely ill patients that have been treated in our intensive care unit over the last 19 years.
At the moment our patients are being treated in a tiny cramped department where we can only manage six patients at a time.
A few months ago, building was started on our new state-of-the-art 24-bed intensive care department. We are hoping to move into our new department at the beginning of 2023.
With the help of Hashem, may my wonderful staff continue to provide the highest level of care to our most complex patients, treating each and every one of them as if they were close family members, helping them and their loved ones negotiate these trying times.
This is an example of the thousands of stories from severely ill patients that have been treated in our intensive care unit at Laniado Hospital over the last 19 years.
At the moment our patients are being treated in a small cramped department where we can only manage six patients at a time.
A few months, ago building was started on our new, state of the art, 17 bed, intensive care department. We are hoping to move into our new department at the beginning of 2023.
With the help of Hashem may my wonderful staff continue to provide the highest level of care to our most complex patients, treating each and every one of our patients as if they are a close family member, helping them and their families negotiate these most dangerous and trying times, safely.
Other News
Celebrating 50 Years of Life: Laniado Hospital’s Golden Birthday

Off-Duty Police Officer Allegedly Stabs Man in Netanya; Victim Treated at Top-Rated Laniado Hospital

A Birth Surrounded by Care, Calm, and Heart at Laniado Hospital



